Exercise During Pregnancy

Exercise for a healthy pregnancy
Benefits
Overall, exercise is a key part of a healthy pregnancy and should be encouraged. Exercise is associated with a reduced risk of certain complications in pregnancy such as gestational diabetes, excessive weight gain, hypertensive disorders, preterm birth, and low birth weight, and may be associated with a reduced risk of cesarean section. It is also associated with a higher incidence of vaginal delivery. Additionally, exercise conveys benefits in the postpartum period by reducing recovery time and preventing postpartum depression. Keep in mind that modifications of various exercises may be necessary due to the physiologic changes of pregnancy, as well as your changing body. Despite what some may have thought in decades past, physical activity in low risk pregnancies is not linked to miscarriage, poor fetal growth, musculoskeletal system injury, or preterm delivery.
Starting an Exercise Routine in Pregnancy
If you are just starting an exercise routine in a low-risk pregnancy, you should be sure to have a thorough clinical exam prior to ensure no medical contraindications. Beginning an exercise routine while pregnant can be intimidating and challenging. You may note body changes and discomfort, a lack of time, and not having a social group or support system for exercising may make starting an exercise routine difficult. Just know that those who are able to incorporate exercise into their prenatal routine have an improvement in well-being, quality of life, and mood. You may also find that you experience fewer episodes of nausea, vomiting, and fatigue. Finally, there is a reduced odds of developing prenatal depression. To get started, set a goal of 20 to 30 minutes daily on most days of the week, aiming to reach 150 minutes of moderate intensity aerobic activity per week during pregnancy and postpartum. A good gauge of “moderate intensity” exercise is the “Talk Test” (Can you carry on a conversation while exercising? If so, than typically this level of activity would not be associated with over-exertion).
Some good options include the following
Yoga, pilates, brisk walking or jogging (outdoors or on a treadmill), cycling (on a stationary bike or outdoors), hiking, water aerobics, swimming, light yard work, ballroom dancing, stretching, strength training and resistance exercises (weights or elastic bands)
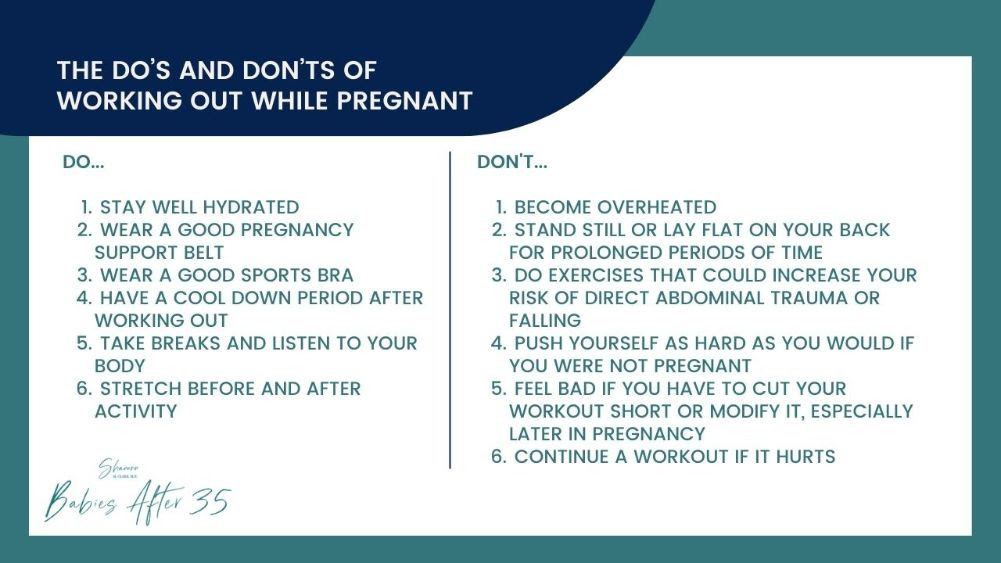
️Those With an Established Exercise Routine
Those with an established, regular exercise routine prior to pregnancy and who have uncomplicated pregnancies, should be able to participate in and maintain the same level of intensity during their pregnancy with no adverse effects, and monitoring your heart rate is not necessary. Be sure to listen to your body and make changes to exercise routines to accommodate the growing uterus, and pay attention to the physiologic fatigue of pregnancy and any limitations on the physical ability for more intense exercises as your pregnancy progresses. Elite athletes are defined as having several years’ experience in a particular sport, usually training 2 times per day, at least 5 days a week. Close monitoring of body temperature, hydration status, and nutrition intake to avoid hypoglycemia during exercise and overall weight loss during pregnancy is recommended, as fetal growth can be affected. Elite athletes are at added risk for activity-related injuries in pregnancy, largely due to compensatory measures taken to counterbalance a changing anatomy, such as pelvic instability or postural changes.
Risks and When to Stop Exercising
Progressive curvature of the lower spine inward, also known as lordosis, during pregnancy leads to increased force on the joints and spine with back pain occurring in 60% of pregnancies. The good news is that abdominal and back muscle strengthening reduces this risk. A supine position (or laying flat on your back) when you are over 20 weeks pregnant may lead to decreased venous return to your heart and a drop in your blood pressure. Be sure to use position modifications for supine activities after this point. Because you lose both water and electrolytes when sweating, be sure to stay adequately hydrated. It can also help to avoid high heat and humidity (especially during the first trimester), and wear loose fitting clothing. Discontinue an exercise program if you experience any of the following and talk to your ObGyn immediately: Vaginal bleeding, abdominal pain, uterine contractions or cramping, amniotic fluid leakage, dyspnea (shortness of breath) before exertion/dizziness, headaches, chest pain, muscle weakness affecting balance, calf pain/swelling, heart palpitations (irregular heart beat).
** Again always discuss your exercise routine with your doctor and obstetrical care provider to see if any modifications should be done or additional fetal surveillance should be initiated. **
